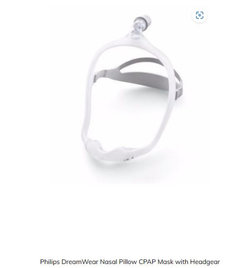
Tell Me About CPAPs
chisue
last year
Featured Answer
Sort by:Oldest
Comments (78)
Elmer J Fudd
last yearLars
last yearlast modified: last yearRelated Discussions
Show me or Tell me about your Shaws Fireclay Sink Flange
Comments (0)Do you have a Shaws Fireclay Sink with an Extended Flange with a garbage disposal? Does yours look thin? Does food lodge around its edge and the Shaws sink flange cut-out?...See MorePlease show me or tell me about your favorite
Comments (5)jxbrown, fwiw, I bought a bunch of those to put on my oven racks. Yes, they do work...but they were a PAIN! I could no longer slide things on/off the shelf. I found them to be impractical...jmho!!! I don't care for mitts, either. Or the silicone pad. I just like the good old-fashioned terry cloth pot holder. I bought some newer quilted ones (not terry) that won't bend easily enough to grip the pan! LOL! I'm always on the search for terry cloth potholders. I must be in the minority since I have a hard time finding them. Here is a link that might be useful: This one is round, but it's the texture I like...See Moreshow me/tell me about your niche/shelf over your range
Comments (11)There was a thread on this topic some months ago--see below. There are some good photos of niches. Our project is bogged down, but I have a few additional comments since I posted... Because we have to watch our pennies, I'm shopping in bargain places. One problem I have encountered is that oddball lots of tiles often don't include bullnose pieces as well as regular field tile sizes. The niche that we have roughed in will require some cute tricks to make ordinary tile edges seem attractive and classy; we don't want to just snip tiles and leave raw edges. DH, my sweaty equity, did not finish the niche smoothly when he created it in drywall because we knew we would cover it in tile. Now, we're thinking that we might not do the tiling right away and he'll have to pull out drywall tools and make a proper corner edging around the niche. This kind of "go back and do over" gig is getting very frustrating. [Meanwhile, I've found a smashingly exciting tile that of course only comes without trim pieces. It's sitting right next to me, thinking. Unfortunately it has a decidedly unfinished raw edge and will require tricky handling if we choose to use it. I just covered it over so I can't see it tempting me there on the table. Have to be more practical. ] Tile shops do carry a metal edging that can be used to finish off edges when no bullnose is available, but I haven't seen examples of it in actual use on a range niche. Would love to see a sample photo to reassure me. Also, remember that if you choose to work with a thick tile or a remnant of some kind of rock from countertop on the back of the niche, that will cut down the depth of the niche shelf. If you want the area above range/cooktop to be an artistic focal point, I humbly suggest that you either make a niche OR some kind of tile design but not both. If you choose too fancy a niche back, the items standing within the niche will compete with the tile design for viewer's attention. Mine will be a working kitchen, so we're planning to put oil bottles, vinegar bottles, salt shaker, etc. there and they are supposed to get top billing. Don't forget that you can suspend a second shelf in the niche if there's room. Here is a link that might be useful: Niche topic thread...See MoreAlternatives to Cpap machine?
Comments (30)Sister has a CPAP machine and it took a long time for her to get used to it period more like months than weeks. She has blood pressure problems but gets a slightly better sleep with a CPAP so the front blood pressure is under control. Just to an aside she also has atrial fibrillation and that causes her to have a buildup of moisture everywhere including in her lungs. So with her doctor's permission she does not use any moisture it her CPAP otherwise she ends up with lung problems and a great deal of settled moisture. That small adjustment has made it so that she does not get pneumonia or bronchitis or shortness of breath as frequently as before. In fact she just doesn't get those infections that she was getting for quite a while. I found out because I asked about it. She did not question anything about anything which is her nature. Good luck on finding an alternative that works for you. Or alternatively a way to get comfortable with it....See Morechisue
last yearAnnie Deighnaugh
last yearlast modified: last yearElmer J Fudd
last yearlast modified: last yearPatriciae
last yearbragu_DSM 5
last yearElmer J Fudd
last yearLindsey_CA
last yearlast modified: last yearAnnie Deighnaugh
last yearOlychick
last yearlast modified: last yearLars
last yearchisue
last yearRNmomof2 zone 5
last yearOlychick
last yearPatriciae
last yearElmer J Fudd
last yearfoodonastump
last yearElmer J Fudd
last yearfoodonastump
last yearnhbaskets
last yearAnnie Deighnaugh
last yearlast modified: last yearmaire_cate
last yearAnnie Deighnaugh
last yearmaire_cate
last yearlast modified: last yearLindsey_CA
last yearAnnie Deighnaugh
last yearOlychick
last yearlast modified: last yearmaire_cate
last yearOlychick
last yearmaire_cate
last yearchisue
last yearRNmomof2 zone 5
last yearElmer J Fudd
last yearlast modified: last yearRNmomof2 zone 5
last yearElmer J Fudd
last yearPatriciae
last yearlast modified: last yearmaire_cate
last yearmaifleur03
last yearjlsch
last yearlast modified: last yearAnnie Deighnaugh
last yearmaire_cate
last yearchisue
last yearElmer J Fudd
last yearchisue
last yearlast modified: last yearElmer J Fudd
last yearLindsey_CA
last yearAnnie Deighnaugh
last year
Related Stories

KITCHEN DESIGNHouzz Call: Tell Us About Your First Kitchen
Great or godforsaken? Ragtag or refined? We want to hear about your younger self’s cooking space
Full Story
FUN HOUZZHouzz Call: Tell Us About Your Dream House
Let your home fantasy loose — the sky's the limit, and we want to hear all about it
Full Story
BATHROOM MAKEOVERSHouzz Call: Tell Us About Your Bathroom Remodel!
Did you recently redo your bath? Please tell us about your upgrade and what it took to get there
Full Story
HOUZZ CALLTell Us: What Puzzles You About Holiday Lights?
Share your questions about and strategies for holiday lights with the Houzz community
Full Story
HOUZZ CALLTell Us About the People You Want to Thank This Year
Please share stories of those who have given you kind words or done deeds that helped you through 2017
Full Story
FEEL-GOOD HOMEGuys Tell Us About Their Favorite Places at Home
For Father’s Day, Houzz men show us the places in their homes where they like to hang out
Full Story
DENS AND LIBRARIES7 Libraries That Tell a Story About the People Who Read There
Book lovers show off their collections in rooms with a range of colors, styles and seating spots
Full Story
FALL GARDENINGWhat Monarch Butterflies Taught Me About Garden Design
Thinking like a butterfly leads to fresh perspectives in the garden and in life
Full Story
COFFEE WITH AN ARCHITECTWhat My Kids Have Taught Me About Working From Home
Candy and Legos aren't the only things certain small people have brought to my architecture business
Full Story





Annie Deighnaugh