Does this seem right (health related)?
debo_2006
14 years ago
Related Stories

HEALTHY HOMEGet Your Light Right for a Healthy House
Homes that are too bright at night and too dark during the day are ruining our health. Here's what you can do
Full Story
INSIDE HOUZZHow Much Does a Remodel Cost, and How Long Does It Take?
The 2016 Houzz & Home survey asked 120,000 Houzzers about their renovation projects. Here’s what they said
Full Story
SMALL SPACESHow to Make Any Small Room Seem Bigger
Get more from a small space by fooling the eye, maximizing its use and taking advantage of space-saving furniture
Full Story
FEEL-GOOD HOMEDoes Your Home Make You Happy?
How to design an interior that speaks to your heart as well as your eyes
Full Story
LIFEThe Polite House: On Dogs at House Parties and Working With Relatives
Emily Post’s great-great-granddaughter gives advice on having dogs at parties and handling a family member’s offer to help with projects
Full Story
DECORATING GUIDESSet the Right Mood With the Right Lines
Soothe with curves or go straight-up efficient. Learn the effects of lines in rooms to get the feeing you’re after
Full Story
KITCHEN DESIGNHouzz Quiz: What Kitchen Countertop Is Right For You?
The options for kitchen countertops can seem endless. Take our quiz to help you narrow down your selection
Full Story
LANDSCAPE DESIGNThe Right Stone for Your Garden Design
Gravel, pebble, cobble and paddle: Stones vary in size and shape, and have different uses in the landscape
Full Story
HOME OFFICESStand-Up Desks Rise to Health Challenges
Sitting all day may be wrecking your health. Are you going to stand for that?
Full Story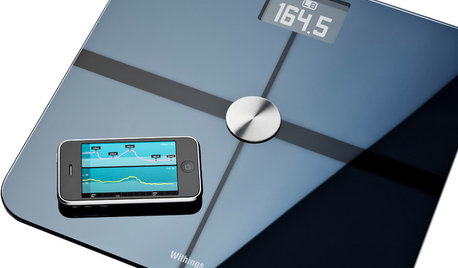
HOME TECHGadgets Help You Watch Your Health at Home
See the crop of new devices that can monitor your body's vital signs and environment for health, fitness and fun
Full Story

mariend
carla35
Related Discussions
looking for a health-related website/forum where you...
Q
Does Number of Litters Affect a Cat's Health?
Q
Water in basement... baffled... seems plumbing related
Q
Does anyone want to help us design our back deck/related landscape?
Q
Vickey__MN
trinitytx
organic_donna
susanjf_gw
debo_2006Original Author
yayagal
carol_in_california
Terri_PacNW